REGIONAL PLAN ASSOCIATION
Key Facts
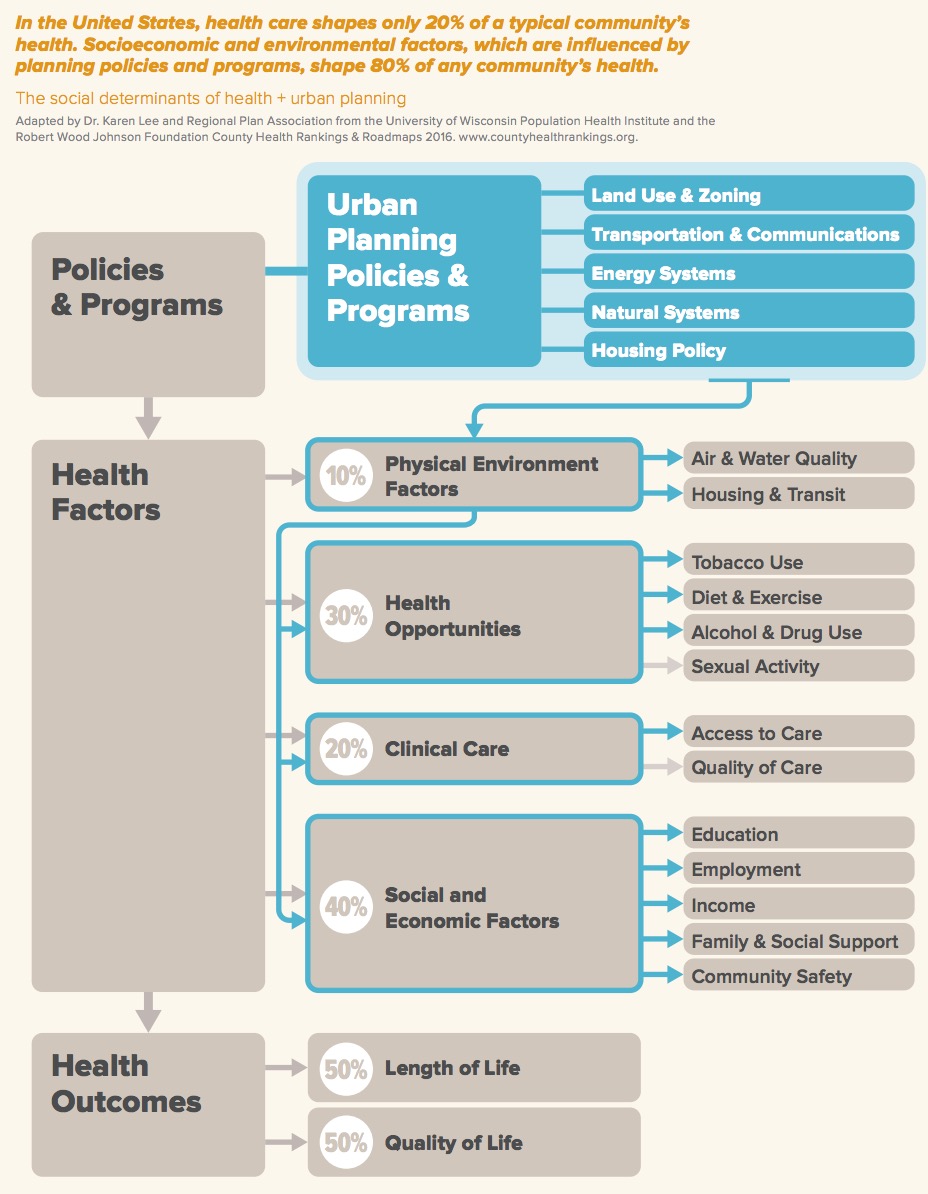
- Health care shapes only 20% of a community’s health in the U.S. Socioeconomic and environmental factors shape 80% of any community’s health.
- People in the region are living longer. In 1990, men’s life expectancy was 71, by 2010 it had increased to 78. In 1990, women’s life expectancy was 78, in 2010 it was 83.
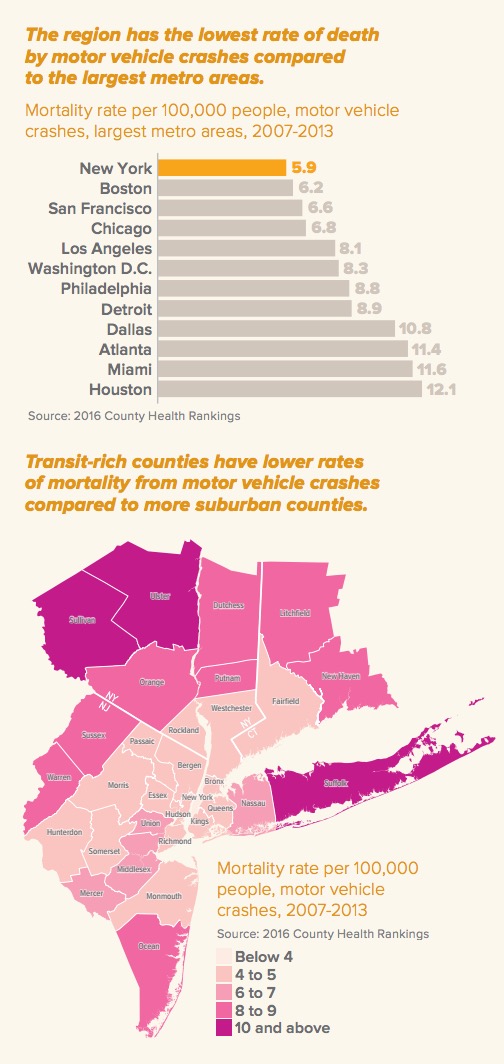
- The region’s urban form, walkability and connectivity can be a health advantage. For example, there are six deaths per 100,000 in the region due to motor vehicle crashes, a third of the national rate.
- There is room for improvement when it comes to quality of life. A typical adult reports 3.4 mentally bad health days & 3.5 physically bad health days per month in the region, higher than several comparable metros.
- There also are big disparities in health between different communities in the region. Life expectancy for blacks is 4-7 years shorter than for whites and Hispanics. Men in Morris County, New Jersey live six years longer than those in neighboring Essex County.
- Inequality and segregation contribute to health disparities. For example, Hispanic children are twice as likely to live in areas with high air pollution as white children.
- Health care costs have increased sharply in recent decades. Health care spending in Connecticut, New Jersey and New York tripled between 1991 and 2009 from 92 billion to 259 billion dollars annually.
Executive Summary
 How do we measure the success of a large metropolitan region? The New York metropolitan region, with its 23 million people living in cities, suburbs, villages and rural communities stretching from New Haven in Connecticut to Ocean County in New Jersey, is larger than most states. Typically when we want to measure a region’s success, we look at the size of its economy, how many jobs and how much wealth it is creating, and how these are distributed among rich, poor and middle class people. We survey residents on how satisfied they are with their community. We measure our air and water quality, housing costs and taxes. We try to capture how good our quality of life is with opinion polls and indexes that attempt to measure and weight factors from the cost of living and educational attainment to climate.
How do we measure the success of a large metropolitan region? The New York metropolitan region, with its 23 million people living in cities, suburbs, villages and rural communities stretching from New Haven in Connecticut to Ocean County in New Jersey, is larger than most states. Typically when we want to measure a region’s success, we look at the size of its economy, how many jobs and how much wealth it is creating, and how these are distributed among rich, poor and middle class people. We survey residents on how satisfied they are with their community. We measure our air and water quality, housing costs and taxes. We try to capture how good our quality of life is with opinion polls and indexes that attempt to measure and weight factors from the cost of living and educational attainment to climate.
But rarely do we take stock of our collective health, perhaps the most fundamental expression of quality of life. And there are good reasons to do so. Disparities in health outcomes are an important way to measure the human cost of inequality. Social and physical environments—such as opportunities for education, employment, active transportation and affordable housing—have been shown to play key roles in improving health. Deliberately incorporating health into how we plan our physical environment can deliver better health outcomes, while expanding our economy and protecting our environment.
This would not be the first time urban planners addressed health. The modern beginnings of urban planning were largely a response to the public health crises facing growing industrial cities in the early 20th century. Preventing the spread of infectious disease epidemics and improving the deplorable living conditions associated with these epidemics was the major challenge of the time. And urban planning achieved marked success, building public services such as sanitation and water systems and containing outbreaks of infectious diseases. Today, we are facing new health challenges: chronic diseases such as heart disease, cancers and diabetes. And just as in the past, an alliance between health professionals and urban planners can be transformative to public health.
Why plan regionally?
This report seeks to add to our understanding of the health impacts of long term urban planning decisions. How do planning decisions such as investment in a subway line, the creation of a park or the redevelopment of a neighborhood affect health outcomes decades later? To answer that question we need to look at not only how individual localities work alone, but how clusters of cities, towns and villages work together.
The New York region spans across three states and includes more than 700 municipalities that are inextricably linked by multiple factors. The local economy and job market is regional in scope, as is the housing market—housing demand in one part of the region will impact prices in another part. The region is connected by a metropolitan transportation system, and other critical infrastructure systems crossing municipal boundaries. The region’s floodplain is part of the shared ecology of the New York Harbor and the Hudson River. These metropolitan systems shape the conditions needed for good health, from the quality of the air we breathe to the types of homes and communities we live in.
RPA’s Fourth Regional Plan, a 25-year blueprint for the built and natural environment in the New York region, can serve as the backbone for such alliances. It is a unique opportunity to transform the region—to create a built environment that eliminates health disparities and provides the basis for good health for all. It is also an opportunity to foster a culture of health by institutionalizing health into planning and by serving as a model for regional plans across the nation.
This report is intended to provide an overall assessment of key health issues in the region today and to identify the key regional systems that play a role in determining health. This, in turn, will inform the recommendations of the Fourth Regional Plan.
The influence of our built and natural environment on health is often poorly understood.
Health is often seen as the product of the health care that people receive as well as their individual decisions concerning diet, smoking, exercise or other such behaviors. Yet the places where we live, work and play are now known to have a profound impact on our overall health and well-being, as well as on the ability to make healthy lifestyle decisions. For example, residents from communities with higher levels of air pollution are more susceptible to a host of illnesses, from respiratory diseases to cancer. Cities and towns with safer streets have fewer traffic-related injuries. The way that our neighborhoods are designed and how easy or difficult it is to walk to work, school, stores, parks and public transportation affects how much physical activity we get. Lack of healthy food options and exposure to unhealthy foods have been shown to be associated with low dietary quality in adults and children.
The influence of our built and natural environment extends beyond these direct impacts. Research by University of Wisconsin Population Health Institute and Robert Wood Johnson Foundation indicates that 80% of population health outcomes are determined by social and economic factors such as income, education or family and social support as well as environmental factors such as walkability or access to services. Their research also shows that these determinants of health vary widely by region and county. Much of the place-based disparity is due to differences in demographics and regional economies. But a growing body of research also shows that the location of affordable housing, the availability and quality of public transportation, and the accessibility of public services all play a large role in education outcomes, economic mobility and other social and economic determinants of health.
Download full version (PDF): How the New York Metropolitan Region’s Urban Systems Influence Health
About the Regional Plan Association
www.rpa.org
RPA is America’s most distinguished urban research and advocacy organization. RPA works to improve the prosperity, infrastructure, sustainability and quality of life of the New York-New Jersey-Connecticut metropolitan region.
Tags: Public Health, Regional Plan Association, RPA, Walkability





 RSS Feed
RSS Feed