Written by James Hinton
This month an opinion piece came out on the Forbes website proposing that telemedicine’s day has come. The piece, written by venture capitalist Skip Fleshman, basically predicts that 2015 will be the year that remote interactions between medical professionals and patients become not just possible, but practical. “I spend a lot of time crisscrossing the country chatting with leading healthcare providers and insurers about their technology needs,” he writes. “By far the area they are most interested in is telemedicine.”
He then goes on to describe why 2015 is the year he expects this interest to see actualization. Internet speeds are up. Mobile devices are everywhere. Health records are finally being digitized. Most importantly, there is a demand for it.
Telemedicine is not a new idea. The idea of a fully integrated medical structure that can bring all of the benefits of advanced medicine to all corners of the world has been a goal for decades. The American Telemedicine Association was founded back in 1993 with the goal of using telemedicine to “improve quality, access, equity and affordability of healthcare throughout the world.”
On their website the ATA directly describes the benefits. Telemedicine can allow primary care providers to consult in real time with specialists through video feeds, the transfer of diagnostic imaging, and vital signs. Remote monitoring can allow medical personnel to monitor patients at work or home, collecting vital sign data in real time to allow long term diagnostics without disruption. Patients can research medical issues and use e-mailed questions to quickly get answers to questions, freeing both doctor and patient from wasting time on unnecessary appointments. Even health education for medical professionals has become more accessible via Internet technologies.
Even futurists are on board with this. Robotic surgery is already commonplace these days. Currently, though, these surgeries are still conducted with the surgeon in the same room as the equipment. In 1964 Futurist and sci-fi writer Arthur C. Clarke stated “I am perfectly serious when I suggest that one day we may have brain surgeons in Edinburgh operating on patients in New Zealand.” The first operation of this sort occurred on September 7th, 2001 when a surgeon in New York used the ZEUS Robotic Surgical System to perform a cholecystectomy on a patient in Strasbourg, France. This has led to predictions that remote surgery will soon become commonplace.
So far, the only area that this promise is being born out in is that of education. The general population with Internet access can use websites such as Web MD or Healthline to learn about health issues they are facing without the need for a doctor’s visit. For rural health care providers a number of respected medical schools are offering advanced coursework online, such as Maryville University or the University of Florida.
The question, however, is whether or not the rest of Fleshman and the ATA’s predictions can come true this year. In order for telemedicine to become widespread and reap large scale benefits the necessary infrastructure has to already be in place. Unfortunately for Fleshman, and for the rest of us, if 2015 is the year that Telemedicine really lands, it won’t be landing in the U.S.
The people who stand the most to gain from Telemedicine are, unfortunately, the ones least likely to have the infrastructure needed for it. The CDC issued a report two years ago highlighting the various disparities in healthcare access by population groups in the U.S. In no surprise the report revealed that when viewed as groups, a number of factors reduced the availability of healthcare access. The factors that were most likely to reduce access included race/ethnicity, sex, education level, economic status, geographic location, and age.
A recent survey conducted by the Census bureau reviewing Internet access may as well be a carbon copy of that same report. African-Americans were 15% less likely to have access to high-speed Internet than Caucasians. Amongst the elderly, access was 25% lower than amongst individuals in their prime. Rural populations had nearly 15% less access than city-dwellers. People below the poverty line were almost 50% less likely to have any Internet access at all than households with an income of $100,000 a year had access to high-speed Internet. Amongst educational levels, individuals with a bachelor’s degree were 30% more likely to have high-speed access than those who had a high school degree only.
This reflects the simple fact that IT Infrastructure follows the money. The money-making formula is simple: the more people you can tie in for the least amount of infrastructure outlay you spend, the higher the profits. Areas that are either low population or which struggle with reduced economic strength provide far less return on investments, which means infrastructure upgrades and maintenance are low priority.
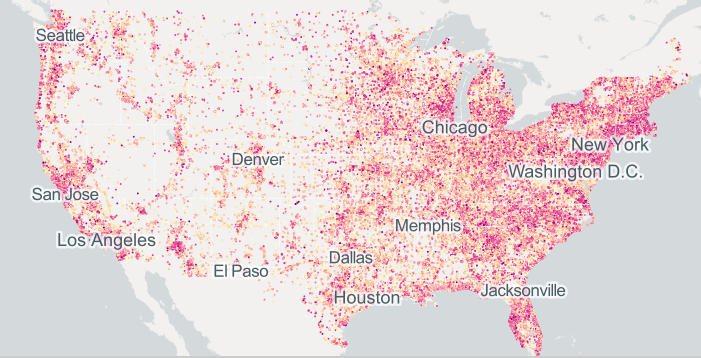
The above map, provided by BroadbandMap.gov, displays the distribution of Internet access speeds throughout the continental U.S. This is not a map of who is using the Internet, but how fast the Internet speeds are for those who do access it. Just like the reports from the Census Bureau and the CDC, Internet access with the speeds necessary to deliver on the promise of telemedicine remains concentrated in those regions most likely to have higher rates of medical access to begin with. For rural regions like the Midwest and Great Basin, or minority-rich areas such as the Lower Mississippi and Southwest, the Infrastructure remains tantalizingly out of reach.
Fleshman’s prediction is one that is full of promise for America’s health access. Telemedicine has the ability to provide rural communities access to specialist care without hours of drive or flight time. For minority populations, access to basic health knowledge can be just an e-mail away. For the poor, longitudinal health tracking doesn’t require extensive periods out of work being hooked up to lab equipment, but instead the chance to have vital statistics monitored even as they put bread on the table. But as things currently stand the potentially life-saving infrastructure needed simply isn’t there.
…
James Hinton is a lifelong learner and army veteran. The son of an engineer, he keeps a close eye on the solutions engineering is developing for future growth.
Tags: Healthcare, James Hinton, Jim Hinton, Rural, Telemedicine





 RSS Feed
RSS Feed
Fantastic article–telemedicine is definitely the future, and thanks to the development of EMR and the healthcare informatics field, the future is NOW!
The argument could be made that informatics is essentially the new telemedicine; everything from access to delivery of healthcare is being digitized and streamlined, and it is breaking down the limitations of geography.
Broadband internet is only the tip of the iceberg that is mobile internet, however–especially when one considers how most of the world outside the US accesses the internet. Telemedicine and informatics are on their way to changing how outbreaks are identified and controlled.
Informatics is definitely a part of the overall package of how telemedicine can bring benefits to everyone, and not just those close to a major hospital. That’s a great point, Edgar.